- All review
Doctors recommend hysteroscopy for many women with intrauterine diseases. What is it? When, why and how is this procedure carried out? Or is it painful? Oresta Marishchuk, reproductologist at the Bogoliuby Center for Reproductive Medicine answers these and other questions that concern our readers.
- What symptoms may indicate intrauterine diseases? What do women with such problems most often complain about?
- Women mainly complain of excessive menstrual flow, significant or minor intermenstrual flow, pain before or during the first days of menstruation, pain during intercourse (this is typical for endometriosis), discomfort during defecation. Common symptoms should also be noted: malaise, weakness, irritability, sudden changes in mood in the period before menstruation. They are less pronounced at a young age and can worsen with age.
- What methods for diagnosing intrauterine diseases currently exist?
- The gold standard for diagnosis is transvaginal ultrasound. If these diseases associated with the cervix, it is necessary to undergo a mirror examination, to do colposcopy (it makes it possible to identify pathological processes in the cervix and cervical canalIn addition, there are such methods of intrauterine diagnosis (and treatment) as diagnostic curettage of the walls of the uterine cavity and hysteroscopy.
- What is hysteroscopy?
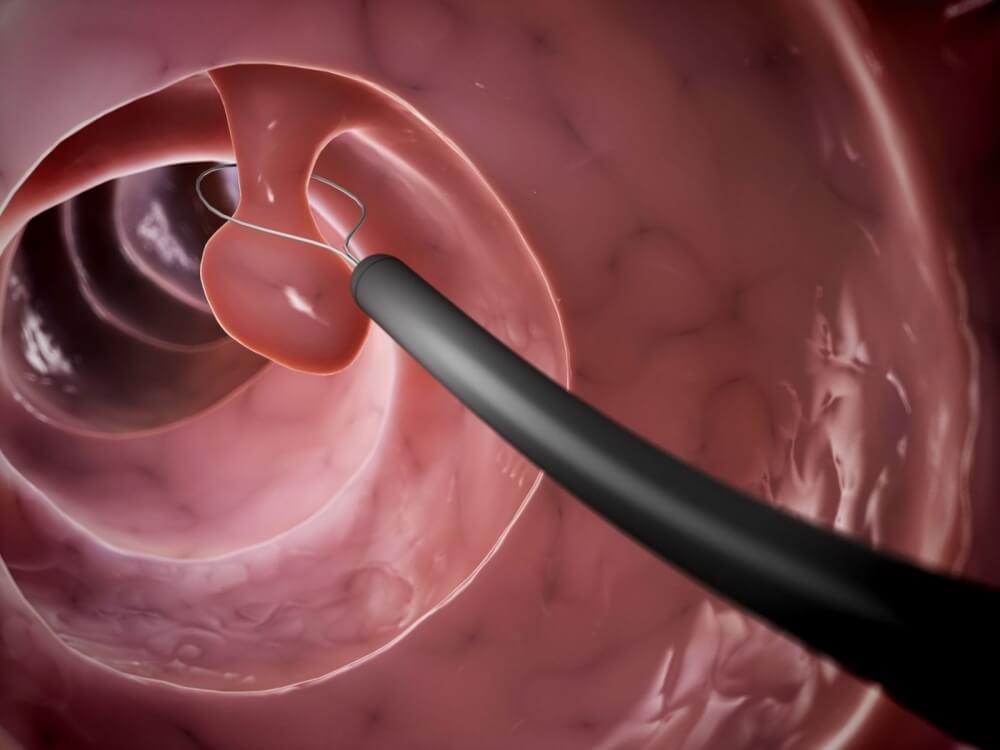
- Hysteroscopy is a method of both diagnosis and treatment. This is the only method that allows you to visualize (examine from the inside) the uterine cavity (with a 20-fold increase), take an endometrial sample for further analysis (histological examination), perform an intrauterine surgical intervention, and also remove the problem areas of the endometrium with a resectoscope. After hysteroscopy and taking into account the results of histology, treatment is prescribed.
- How is this procedure different from curettage?
- Hysteroscopy, in contrast to curettage, is a visual diagnostic method, because during the procedure a hysteroscope is inserted into the uterine cavity - a device that allows you to examine the organ from the inside and see where the pathology is located. The diagnostic procedure may end with treatment - removal of the pathological area from the uterine cavity. Curettage, in contrast to hysteroscopy, is a «blind» procedure - when curettage, a pathological area in the uterine cavity is not visualized. For example, if the uterus has a polyp, hysteroscopy can completely remove it, and during curettage the probability of partial removal, and then the possibility of a relapse of the disease. It should also be noted that hysteroscopy, in which the problem area of the mucosa is taken, is less traumatic than curettage, in which the entire mucosa is injured.
- Who is recommended to undergo hysteroscopy?
- The doctor can refer the patient to hysteroscopy if she has a polyp in the uterus or submucous (submucous) uterine fibroids during ultrasound, when she has intermenstrual bleeding (not related to menstruation), infertility, endometrial hyperplasia, adenomyosis, developmental abnormalities uterus, as well as for monitoring after hormonal therapy due to hyperplastic processes in the uterine cavity. Pathological discharge from the genital tract in postmenopausal women - showing in hysteroscopy. The accuracy of diagnosis of endometrial cancer in postmenopausal women is almost 100%. In this case, it is possible to determine the localization of the process and its prevalence, which is important for the choice of tactics of patient management. If there is a suspicion of the remains of the fetal occyte after an abortion or placental tissue after childbirth, it is very important to conduct a hysteroscopy to purposefully remove pathological tissues without injuring the rest of the endometrium, is a preventive measure for the formation of synechia (adhesions).
- How does the hysteroscopy procedure take place?
- Scheduled hysteroscopy is performed in the first phase of the cycle - on the fifth-seventh, maximum ninth day of the menstrual cycle (i.e. immediately after the end of menstruation, since the endometrium is thin and minimally vascularized). Before the procedure, the patient must be examined, blood group and rhesus blood are determined, checked for syphilis, AIDS, hepatitis B and C, a detailed blood test, coagulation, smears for cancer cells and purity, ultrasound of the pelvic organs are done. Hysteroscopy is performed on an empty stomach, under anesthesia (general intravenous anesthesia), so a woman feels absolutely nothing. No cuts are made during the procedure, because a hysteroscope is inserted into the uterine cavity through the genital tract. The procedure usually lasts 10-15 minutes. There is no pain after hysteroscopy, as a rule, and if there is, then it is easily eliminated by analgesics. With planned hysteroscopy, complications are rare. After completing the procedure, moving away from anesthesia and receiving the recommendations of a doctor, a woman can immediately go home.
- Are there any contraindications for hysteroscopy?
- The procedure is contraindicated in acute infectious diseases (for example, acute respiratory viral infections, pneumonia, tonsillitis), in acute infections of the genital organs, cervical cancer and pregnancy.
- in acute infections of the genital organs, cervical cancer and pregnancy.
- What are the risks of intrauterine diseases if they are not treated?
- At a young age, for example, polyp or hyperplasia, lead to infertility, irregular menstruation. At an older age, intrauterine diseases can lead to excessive and prolonged menstruation, which cause anemia, a violation of the general condition of the patient, as well as a possible degeneration into cancer. Therefore, it is important to regularly undergo medical examinations and timely diagnose and treat diseases.
